PAPOVAVIRIDAE
In the past the polyomaviruses and the papillomaviruses were considered to be two subfamilies within the family Papovaviridae.
However, the mode of replication, genome organization,
and evolutionary history of polyomaviruses and papillomaviruses are
distinct and they are now classified into two distinct families:
Papillomaviridae (50-55 nm)
Polyomaviridae(41-44 nm)
PAPILLOMAVIRIDAE
Naked, circular, dsDNA.
Circular dsDNA represent miniature models for eukaryotic cell DNA.
Heavily dependent on cellular machinery both for replication and gene expression.
Under certain conditions may transform cells in a manner resembling malignancy.
May transform non-permissive host cells and cause papillomas, keratinized skin tumors or warts.
Good model to study the development of cancer (tumor virus oncogenes are very similar to human oncogenes).
Have been found in most mammals and birds.
Highly host specific.
Resistant to ether, low pH and heat.
Structure
The icosahedral virion is 55 nm in diameter.
Spherical protein coat of approximately 72 capsomers.
The major component of the virion is the capsid protein.
It makes up 80% of the total viral protein.
Uncoats and assembles inside cell nucleus.
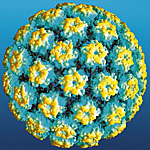
Molecular surface of the atomic model of the
capsid of papillomaviruses
Source: ICTV - Stephen Harrison
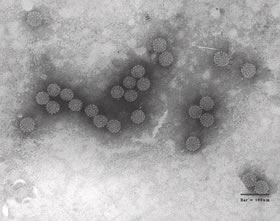
Source: Prof. Steward McNulty, Queen's University, Belfast.
Types of Papillomaviruses
Sixteen currently recognized genera of papillomaviruses have been identified.
Genera are simply named by Greek letters.
Alphapapillomavirus, Betapapillomavirus and Gammapapillomavirus contain the 96 types that affect humans.
Types are very specific for different epithelia (i.e. one type causes warts on hand but not feet).

Viral forms (HPV types 5, 6, 8, 16 & 18) are noted only in the top differentiated levels of common warts.
HPV 16, 18, 31, 33 cause malignant lesions - these are the major cause of carcinomas in humans.
It has been shown that HPV6 and HPV11 cause benign genital warts suppressing protein p53.
p53 coded by TP53 gene. Prevents cancer (genome mutations) - a tumor suppressor protein.
Difference between benign and malignant is probably in the specific cell type they infect.
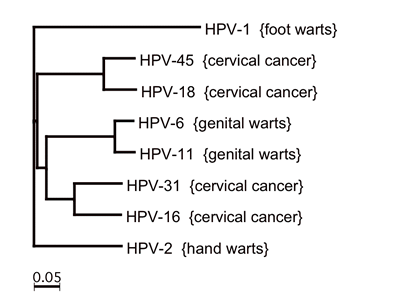
Most common types of papillomaviruses associated with disease.
Types based on nucleotide sequences. HPV1 is a Mupapillomavirusand the remaining belong to genus Alphapapillomavirus.
Source: Parkin, D.M. (2006). Int. J. Cancer 118:3030-44
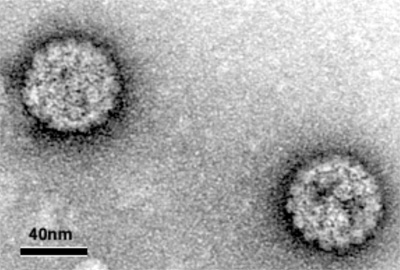
The HPV-16 virus - causes carcinomas.
Source: Helenius Project, Institut fur Biochemie, ETH, Zurich
Genome
It is surmised that their genome is present in plasmid form in the basal cell layer of the skin.
Genome does not express its full viral protein complement until differentiation takes place.
Genome is 8 kb in size.
Types of Papillomaviruses
Sixteen currently recognized genera of papillomaviruses have been identified.
Genera are simply named by Greek letters.
Alphapapillomavirus, Betapapillomavirus and Gammapapillomavirus contain the 96 types that affect humans.
Types are very specific for different epithelia (i.e. one type causes warts on hand but not feet).

Viral forms (HPV types 5, 6, 8, 16 & 18) are noted only in the top differentiated levels of common warts.
HPV 16, 18, 31, 33 cause malignant lesions - these are the major cause of carcinomas in humans.
It has been shown that HPV6 and HPV11 cause benign genital warts suppressing protein p53.
p53 coded by TP53 gene. Prevents cancer (genome mutations) - a tumor suppressor protein.
Difference between benign and malignant is probably in the specific cell type they infect.
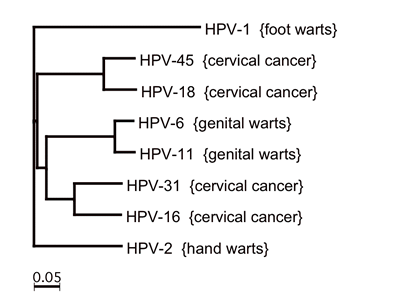
Most common types of papillomaviruses associated with disease.
Types based on nucleotide sequences. HPV1 is a Mupapillomavirusand the remaining belong to genus Alphapapillomavirus.
Source: Parkin, D.M. (2006). Int. J. Cancer 118:3030-44
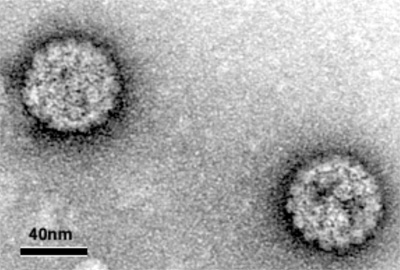
The HPV-16 virus - causes carcinomas.
Source: Helenius Project, Institut fur Biochemie,
ETH, Zurich
Genome
It is surmised that their genome is present in plasmid form in the basal cell layer of the skin.
Genome does not express its full viral protein complement until differentiation takes place.
Genome is 8 kb in size.
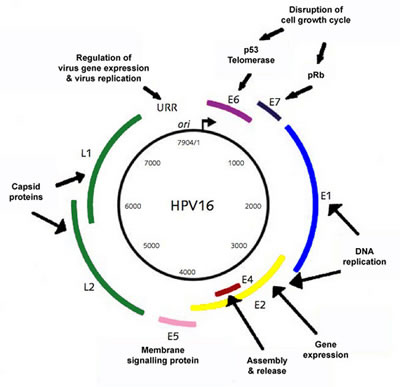
Genome of HPV16 - Late (L1-2) and Early (E1-8) genes or ORF's
Source: Helenius Project, Institut fur Biochemie, ETH, Zurich
Functions
E1 - initiates DNA replication
E2 - transcriptional regulation/DNA replication
E3 - unknown
E4 - disruption of cytoskeleton
E5 - Interacts with growth factor receptors
E6 - binds to p53 (promotes apoptosis)
E7 - binds to pRB (cellular protein that stops proliferation)
E8 - unknown
L1 - major capsid protein
L2 - minor capsid protein
Replication
Tropic for squamous epithelial cells but the receptors are unknown.
E1-E5 genes are expressed right after infection.
These genes encode proteins that regulate viral mRNA synthesis and that are involved in the replication of the genome of the virus.
Only one strand of the genome is transcribed, producing two classes of proteins: the non-structural regulatory proteins, known as early proteins (E), and the structural proteins L1 and L2, known as late proteins.
When the HPV infects the basal cells it produces only a small number of viral genomes, and replicates in parallel with the replication of the basal cell DNA.
At this point the virus does not complete its reproductive program and no capsid proteins produced.
The genetic information of the virus is said to be trapped.
The virus infects the basal cells of the dermal layer, and early gene expression can be detected in these cells.
As basal cells move toward the surface and begin to mature, they become more permissive allowing the virus to change from being a passenger to being in control.
The most confusing thing is that in most cases, all or part of the papilloma genome including the "transforming genes" is maintained in the tumor cells.
E6 and E7 allow the virus to complete its reproductive program in the mature cell.
E6 promotes the degradation of the cellular p53 tumor suppressor (p53 normally triggers apoptosis). Allows cell to continue viral replication -- virus protects the cell from apoptosis.
E7 binds to cellular protein pRB (stops cell proliferation).
The unnatural or abnormal continued proliferation of a mature cell allows the rest of the viral genes to be expressed, and viral replication is continued and completed.
These characteristics allow the virus to replicate undetected by the body's immune system.
Late gene expression -- expression of structural proteins and vegetative DNA synthesis is restricted to terminally differentiated cells of the epidermis.
New virus particles are assembled.
HPV can persist from a few months to a few years.
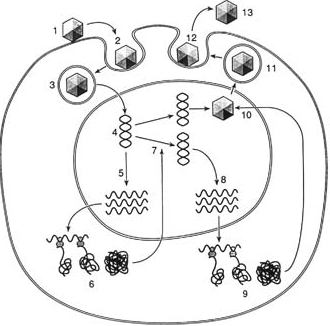
Replication cycle of papillomaviruses Source: Standford University
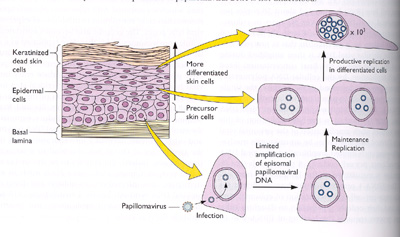
Plasmid (episome) Replication
The virus infects proliferating basal epithelial cells, to which it probably gains access after wounding.
The double stranded circular DNA genome (episome) is imported into the infected cell nucleus and amplified to a concentration of 50 to 100 copies per cell.
This concentration of viral DNA episomes is maintained by further limited replication as the basal and parabasal cells of the epithelium divide (maintenance replication).
As cells move to the outer layers of the epidermis and differentiate, replication of the viral genome to thousands of copies per cell takes place.
The mechanism by which differentiation induces the switch from maintenance to productive replication ofpapillomaviral DNA is not understood.
The DNA of Papillomavirus is rarely, if ever, integrated into the host genome but remains as a circular plasmid (episome) in the nucleus of the transformed cell.
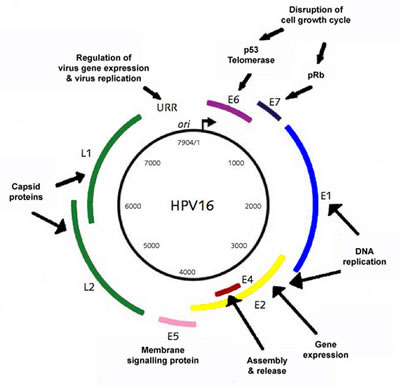
Genome of HPV16 - Late (L1-2) and Early (E1-8) genes or ORF's
Source: Helenius Project, Institut fur Biochemie, ETH, Zurich
Functions
E1 - initiates DNA replication
E2 - transcriptional regulation/DNA replication
E3 - unknown
E4 - disruption of cytoskeleton
E5 - Interacts with growth factor receptors
E6 - binds to p53 (promotes apoptosis)
E7 - binds to pRB (cellular protein that stops proliferation)
E8 - unknown
L1 - major capsid protein
L2 - minor capsid protein
Replication
Tropic for squamous epithelial cells but the receptors are unknown.
E1-E5 genes are expressed right after infection.
These genes encode proteins that regulate viral mRNA synthesis and that are involved in the replication of the genome of the virus.
Only one strand of the genome is transcribed, producing two classes of proteins: the non-structural regulatory proteins, known as early proteins (E), and the structural proteins L1 and L2, known as late proteins.
When the HPV infects the basal cells it produces only a small number of viral genomes, and replicates in parallel with the replication of the basal cell DNA.
At this point the virus does not complete its reproductive program and no capsid proteins produced.
The genetic information of the virus is said to be trapped.
The virus infects the basal cells of the dermal layer, and early gene expression can be detected in these cells.
As basal cells move toward the surface and begin to mature, they become more permissive allowing the virus to change from being a passenger to being in control.
The most confusing thing is that in most cases, all or part of the papilloma genome including the "transforming genes" is maintained in the tumor cells.
E6 and E7 allow the virus to complete its reproductive program in the mature cell.
E6 promotes the degradation of the cellular p53 tumor suppressor (p53 normally triggers apoptosis). Allows cell to continue viral replication -- virus protects the cell from apoptosis.
E7 binds to cellular protein pRB (stops cell proliferation).
The unnatural or abnormal continued proliferation of a mature cell allows the rest of the viral genes to be expressed, and viral replication is continued and completed.
These characteristics allow the virus to replicate undetected by the body's immune system.
Late gene expression -- expression of structural proteins and vegetative DNA synthesis is restricted to terminally differentiated cells of the epidermis.
New virus particles are assembled.
HPV can persist from a few months to a few years.
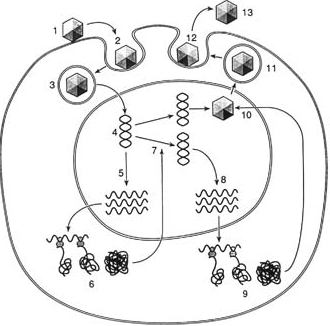
Replication cycle of papillomaviruses Source: Standford University
Plasmid (episome) Replication
The virus infects proliferating basal epithelial cells, to which it probably gains access after wounding.
The double stranded circular DNA genome (episome) is imported into the infected cell nucleus and amplified to a concentration of 50 to 100 copies per cell.
This concentration of viral DNA episomes is maintained by further limited replication as the basal and parabasal cells of the epithelium divide (maintenance replication).
As cells move to the outer layers of the epidermis and differentiate, replication of the viral genome to thousands of copies per cell takes place.
The mechanism by which differentiation induces the switch from maintenance to productive replication ofpapillomaviral DNA is not understood.
The DNA of Papillomavirus is rarely, if ever, integrated into the host genome but remains as a circular plasmid (episome) in the nucleus of the transformed cell.
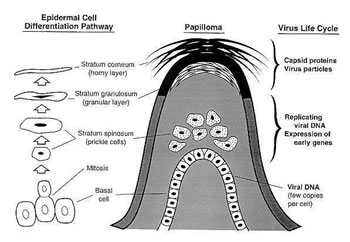
Epidermal cell differentiation and viral replication
Source: Medical Microbiology. UTMB.
Events that occur in the top layers of the skin
Flint et al. 2000. Principles of Virology. ASM
Press.
Human Diseases
Genital Disease and Cancer
HPV can grow on the cervix, vagina, vulva, urethra, penis and the anus.
HPV causes condyloma (warts) and dysplasia (pre-cancer), two kinds of abnormal tissues.
Cervical cancer is the leading lethal malignancy in the world.
HPV16 and HPV18 cause 70% of cervical cancer cases.
In cervical carcinoma, other viruses (e.g., Herpes simplex virus type 2 or human cytomegalovirus) or other infectious agents (e.g., Chlamydia) have been implicated as cofactors with human Papillomavirus 16.
Within the 60 types of HPV types some are associated with benign genital condylomas, others are associated with genital and oral/pharyngeal carcinomas.
HPV 6 and HPV11 cause 90% of genital wart cases.
Multiple sexual partners and early age of first intercourse have been recognized as cofactors.
In epidermodysplasia verruciformis, impaired cell-mediated immune responses and exposure to sunlight are important cofactors.
Genital warts range from almost unnoticeable small bumps to giant, cauliflower-like growths calledcondylomata acuminata; may cause penile cancer.
Non-genital disease
Up to 96 different types of human papilloma- viruses have been identified associated with warts and epidermal and epithelial lesions at different sites.
Some types cause skin warts which are common in school children.
Other types have been isolated from patients with a rare disease called epidermodysplasia verruciformis.
These patients are unable to resolve their warts, probably because of an inherited immunologic defect, and wart-like lessions appear all over the body. These warts often become malignant after many years, especially on areas of the skin exposed to sunlight, but these tumors are generally slow growing and do not metastasize (J.H & E.G. Strauss, 2008).
How papillomaviruses enter and emerge the cell is not known.
Limited in their cell tropism (epithelial cells) and are difficult to grow in tissue culture.
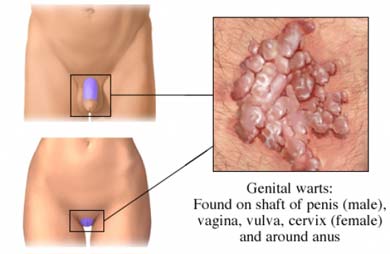
Condylomata acuminata - Genital warts.
Transmission
There is very little information available as to how or when people become infected with HPV.
It is believed to be transmitted through direct contact or fomites.
Incubation from infection to warts is 3-4 months.
Route of transmission appears to be through cracks in the skin or tears in the mucosal barrier.
Use of condoms affords very little protection against infection.
Treatment
Topical medication (podofilox or imiquinod).
Wart removal by cryosurgery, electrocautery, trichloroacetic acid or laser.
Cervical cancer by removal of carcinogenic cells (surgery, radiation therapy orchemotherapy).
Statistics (U.S.A)
25 million Americans are currently infected.
More than one million new cases every year.
It is the second most commonly acquired STD.
40-60% of all college students.
Summary on Human Diseases
Human Papillomaviruses (HPV) is a group of more than 100 types of viruses transmitted through sexualintercourse and may be present in as many as one out of three sexually active young adults.
Although the virus is common in men and women, most people with HPV do not know that they are infected since HPV is usually asymptomatic, that is they cause no symptoms.
The majority of HPV infections go away on their own and do not cause cancer.
Some HPVs can cause the growth of abnormal cells and lead to cancer.
HPV infection of the cervix has been shown to be a cause of cervical cancer.
Animal Papillomaviruses
Have been found in warts from rabbits, hamsters, mice, sheep, goats, deer, cattle, horses, dogs, and monkeys.
Cottontail rabbit Papillomavirus
Bovine Papillomavirus 1, 2 and 4
Canine oral PapillomavirusFeline Papillomavirus
Deer Papillomavirus
Elephant Papillomavirus
Equine Papillomavirus
Ovine Papillomavirus
When transferred to another animal species, they can often cause malignancies.
Detection
DNA hybridization and PCR.
POLYOMAVIRIDAE(poly = many; oma = tumor)
Naked, circular, dsDNA.
Similar to papillomaviruses but smaller.
41 nm diameter.
The most commonly studied member is the simian virus (SV40) that was inadvertently introduced to about 30 million humans in both polio vaccines (Sabin and Salk).
SV40 was found in screening of kidneys of Rhesus monkeys that were used to cultivate the polio virus.
Polyomaviral DNA carries part of the genetic information on each strand, and these can become integrated into the host cell genome.
The DNA by itself is infectious!
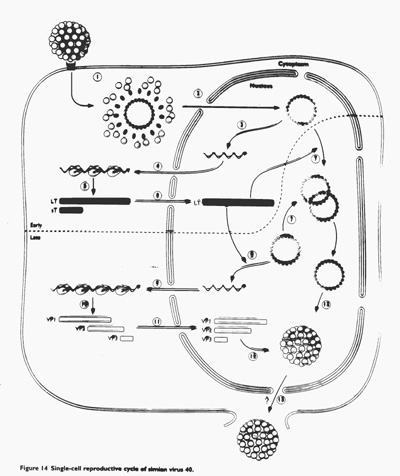
Replication of SV40. Fields et al. 1995. Foundamental Virology. Lw&W.
Genome Expression
The mechanism of gene E6 action is different than that of SV40.
Involves degradation of the cellular p53 tumor suppressor allowing the cell to continue viral replication. p53 is a protein which normally triggers apoptosis in a cell.
Diseases
Cause several different tumors in animals and humans.
Associated with urinary tract infection (BK disease) and a central nervous system demyelinating disease.
Most humans in the USA are infected (latent in kidneys) with the BK virus before the age of 10.
JC virions are possibly latent in the brain.
Both JC and BK were named after the initials of the patients from whom they were isolated.
Most BK and JC viruses are not associated with illness.
Reactivation of both could be brought about by immuno-suppression or by factors such as pregnancy and diabetes.
Cause progressive multifocal leukoencephalopathy (PML).